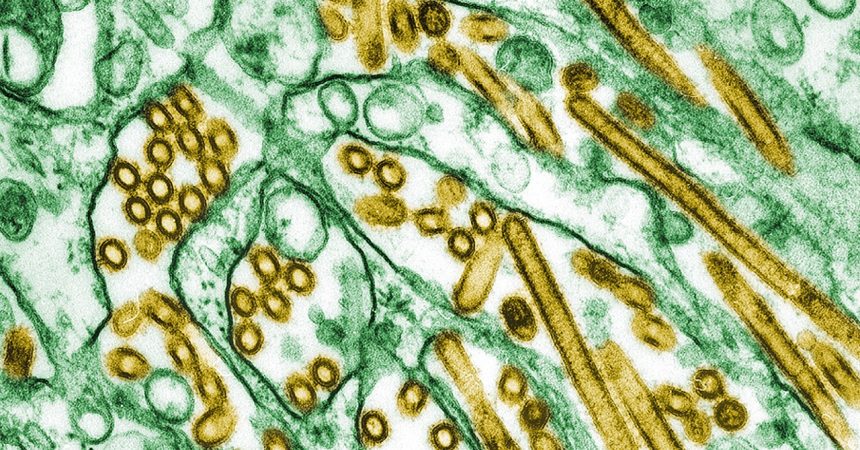
The United States has recently confirmed its first case of severe avian influenza (H5N1 bird flu) in a human, marking a significant development in the ongoing outbreak affecting both animal and human populations. While previous human cases in the US this year have been mild, the hospitalization of a Louisiana resident underscores the potential for H5N1 to cause serious illness. This case differs from earlier infections as the patient’s exposure is linked to backyard flocks, rather than commercial poultry farms, highlighting a new avenue for potential human infection.
The current H5N1 outbreak has had a devastating impact on poultry and wild bird populations across the United States. Over 800 dairy herds in 16 states have been affected, contributing to the spread of the virus to humans who come into close contact with infected animals. Prior to the Louisiana case, 61 human bird flu cases were reported in eight states, primarily among individuals exposed to sick or infected dairy cows or poultry involved in culling operations. These cases presented with mild symptoms, such as conjunctivitis and respiratory issues, and all patients fully recovered.
The Louisiana case raises concerns due to the historical association of H5N1 with severe illness and mortality in other countries. Globally, from 2003 to 2023, H5N1 infections have resulted in a significant number of deaths, with a mortality rate of approximately 50% among confirmed cases. The severity of this recent case emphasizes the need for vigilance and preventative measures, especially for those in close contact with birds. While the immediate risk to the general public remains low, the potential for severe illness necessitates continued monitoring and proactive strategies to mitigate the spread of the virus.
The investigation into the Louisiana case reveals a link between the patient’s exposure to sick and dead birds in their backyard flock and the development of severe H5N1 infection. This is the first instance in the US where a human H5N1 case has been traced back to a backyard flock, as opposed to a commercial farm setting. While the precise details of the exposure and the patient’s current condition remain undisclosed, the link to backyard flocks underscores the importance of preventative measures for individuals maintaining such flocks.
Genetic analysis of the virus from the Louisiana patient reveals similarities to the strain found in a hospitalized teenager in Canada, both categorized as type D1.1. This variant has also been detected in wild birds and poultry in the US. This differs from the B3.13 type, predominantly found in dairy cows, some poultry outbreaks, and sporadic human cases. The identification of the D1.1 variant in the Louisiana case warrants further investigation to understand its potential for increased human infectivity or transmission. Ongoing genomic sequencing will provide crucial insights into any changes in the virus that could signal a heightened risk to human health.
While person-to-person transmission of H5N1 bird flu has not been observed, the Louisiana case highlights the potential for severe illness and the need for continued surveillance and preventative measures. The CDC emphasizes that individuals with occupational or recreational exposure to birds, including backyard flock owners, hunters, and bird enthusiasts, face a higher risk of infection. Therefore, it is crucial for these individuals to take appropriate precautions to minimize their risk of exposure and protect themselves from potential infection. The ongoing investigation and genomic sequencing will provide valuable data to inform public health strategies and mitigate the potential impact of H5N1 on human health.